For the first time ever, a US man has received two kidney transplants from a genetically modified pig.
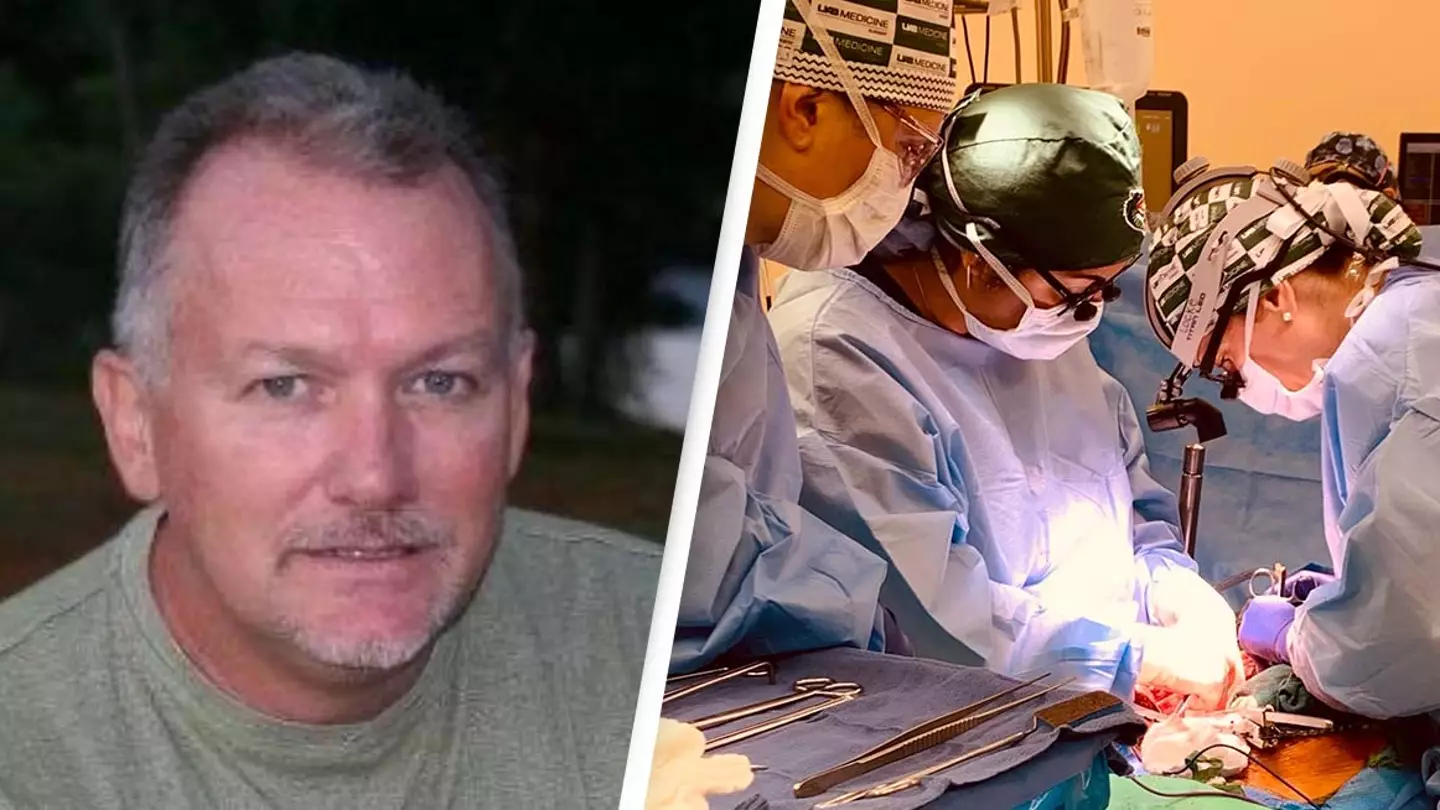
Jim Parsons, 57, was suffering with acute kidney injury and had no prospect of recovery. He was being maintained on a ventilator to keep his body functioning normally. As a registered organ donor, he'd hoped to be able to help others with his organs in the event of his death, but they weren't suitable.
Advert
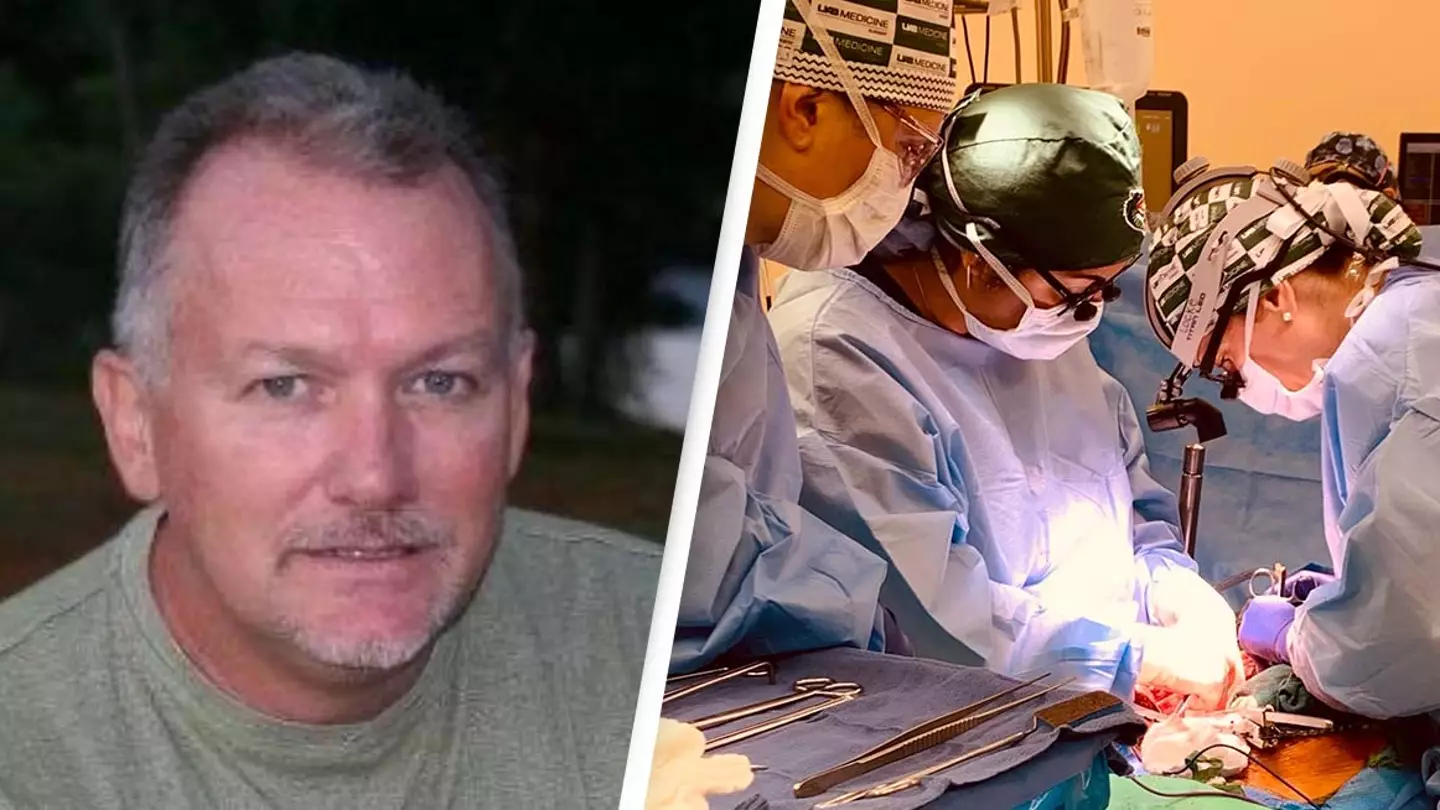
In a breakthrough procedure, two kidneys from a pig were successfully transplanted into Parsons' body. While he was brain-dead, the organs worked for more than three days.

It's hoped this could solve the organ shortage crisis, with people on waiting lists passing away every day. It also comes after David Bennett, 57, became the first person in the world to receive a pig heart. He's said to be doing well after the operation.
'This game-changing moment in the history of medicine represents a paradigm shift and a major milestone in the field of xenotransplantation, which is arguably the best solution. We have bridged critical knowledge gaps and obtained the safety and feasibility data necessary to begin a clinical trial in living humans with end-stage kidney failure disease,' senior author Dr. Jayme Locke, of the University of Alabama at Birmingham (UAB), said.

Parsons' family gave permission for the procedure to go ahead at the university's Legacy of Hope Donor Recovery Centre. The kidneys filtered blood, produced urine and, importantly, were not immediately rejected, and they remained viable until 77 hours after transplant.
Advert
'Mr Parsons and his family allowed us to replicate precisely how we would perform this transplant in a living human. Their powerful contribution will save thousands of lives, and that could begin in the very near future,' Dr. Locke said.
Parsons' ex-wife, Julie O'Hara, also said, 'Jim was a never-met-a-stranger kind of guy who would talk to anyone and had no enemies – none. Jim would have wanted to save as many people as he could with his death, and if he knew he could potentially save thousands and thousands of people by doing this, he would have had no hesitation.'

'Our dream is that no other person dies waiting for a kidney, and we know that Jim is very proud that his death could potentially bring so much hope to others.'
Advert
Xenotransplantation, in which organs from animals are put into humans, has been a goal for scientists for decades. Currently, kidney disease kills more people each year than breast or prostate cancer. 'A radical solution is needed for the organ supply crisis. The domestic pig is a promising organ source,' Dr. Locke said.
As pig heart valves are already widely used in humans, extensive tests on non-human primates with genetically modified pig kidneys have been taking place to ascertain the 'safety and feasibility of the pig-to-non-human primate model, without risk to a living human', she continued.
'Our study demonstrates major barriers to human xenotransplantation have been surmounted, identifies where new knowledge is needed to optimise xenotransplantation outcomes in humans, and lays the foundation for the establishment of a novel preclinical human model for further study,' she added.
If you have a story you want to tell, send it to UNILAD via [email protected]
Topics: US News
