Doctors have revealed a new experimental therapy for patients with pancreatic cancer.
In 2018, Kathy Wilkes, from Ormond Beach, Florida, was diagnosed with aggressive pancreatic cancer.
However, this year, in just a single month, the 71-year-old had her metastic cancer reduced by 50 percent by a 'one-and-done' treatment.
Prior to the new experimental therapy, Wilkes' cancer had been continuing to spread.
Advert
Despite eight rounds of chemotherapy and having part of her pancreas removed in an operation, it took just a year for the cancer to spread to her lungs.
Wilkes told NBC News: "When I talked to my hometown oncologist and asked him what to do, he only had one answer, and that was chemotherapy. And I said, ‘That’s not my answer'.
"I thought, 'That is the trial I want'. I knew that that was the trial that was going to save me, save my life. I just had that feeling."
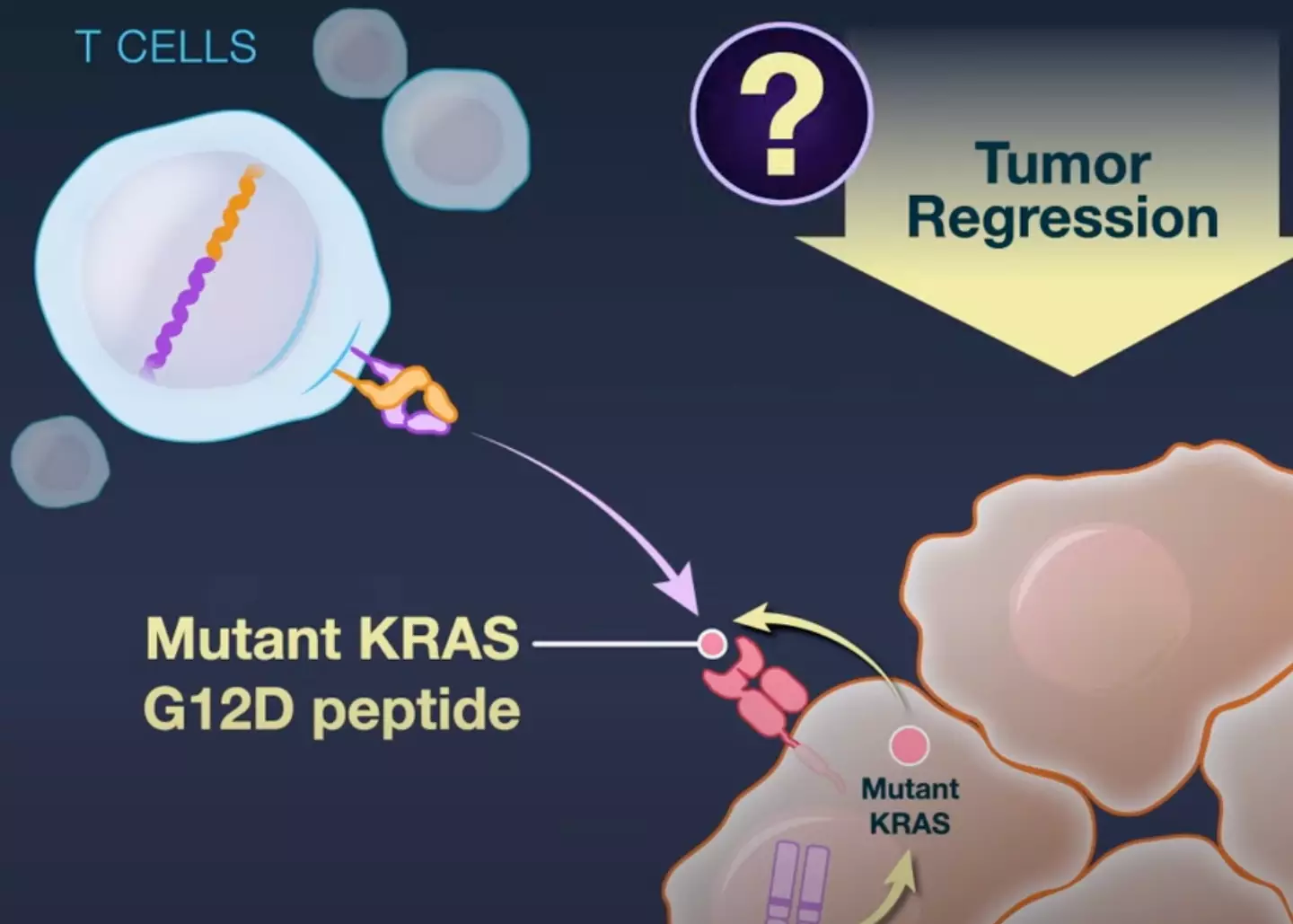
Wilkes subsequently reached out to Dr Eric Tran, who is the author of a report on an experimental type of gene therapy that targets KRAS G12D – a type of cancer mutation.
Advert
She agreed to undergo a new experimental therapy known as Neoantigen T-Cell Receptor Gene Therapy.
Five days before the main treatment, 'the patient received a single flat dose of tocilizumab (600 mg, administered intravenously) in order to prevent cytokine release syndrome, which can occur after the infusion of gene-engineered T cells'.
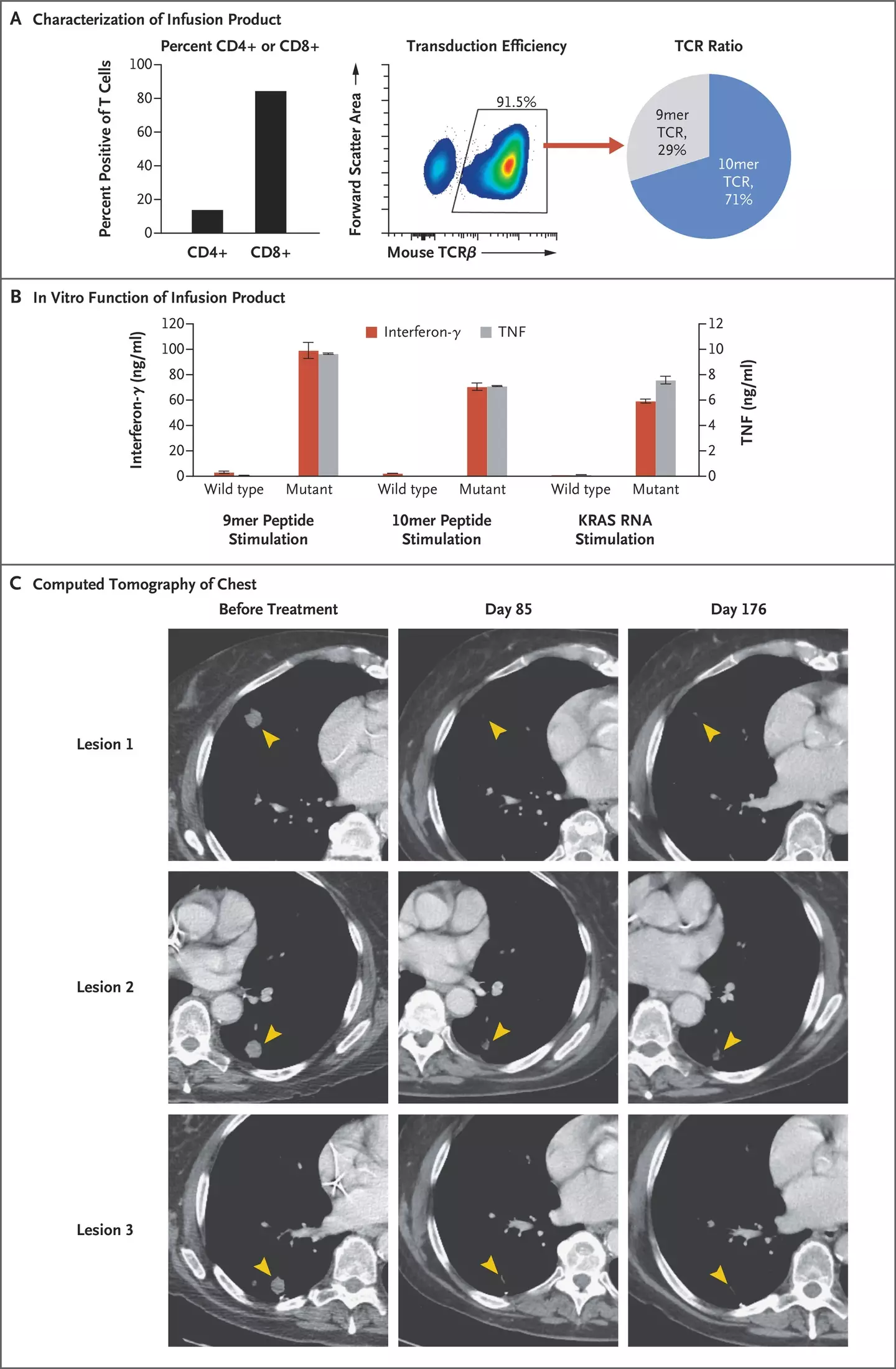
On 'day zero', doctors then treated her progressive metastic pancreatic cancer with 'a single infusion of 16.2×109 autologous T cells, which consisted of 85% CD8+ T cells and 15% CD4+ T cells. [...] Approximately 91.5% of the infusion product (14.8×109 cells) expressed a KRAS G12D–reactive TCR'.
'In order to support the expansion of infused T cells,' Wilkes received 'high-dose interleukin-2 (600,000 IU per milliliter, administered intravenously every 8 hours) for five of the six planned doses' 18 hours after the infusion.
Advert
The sixth dose was not administered.
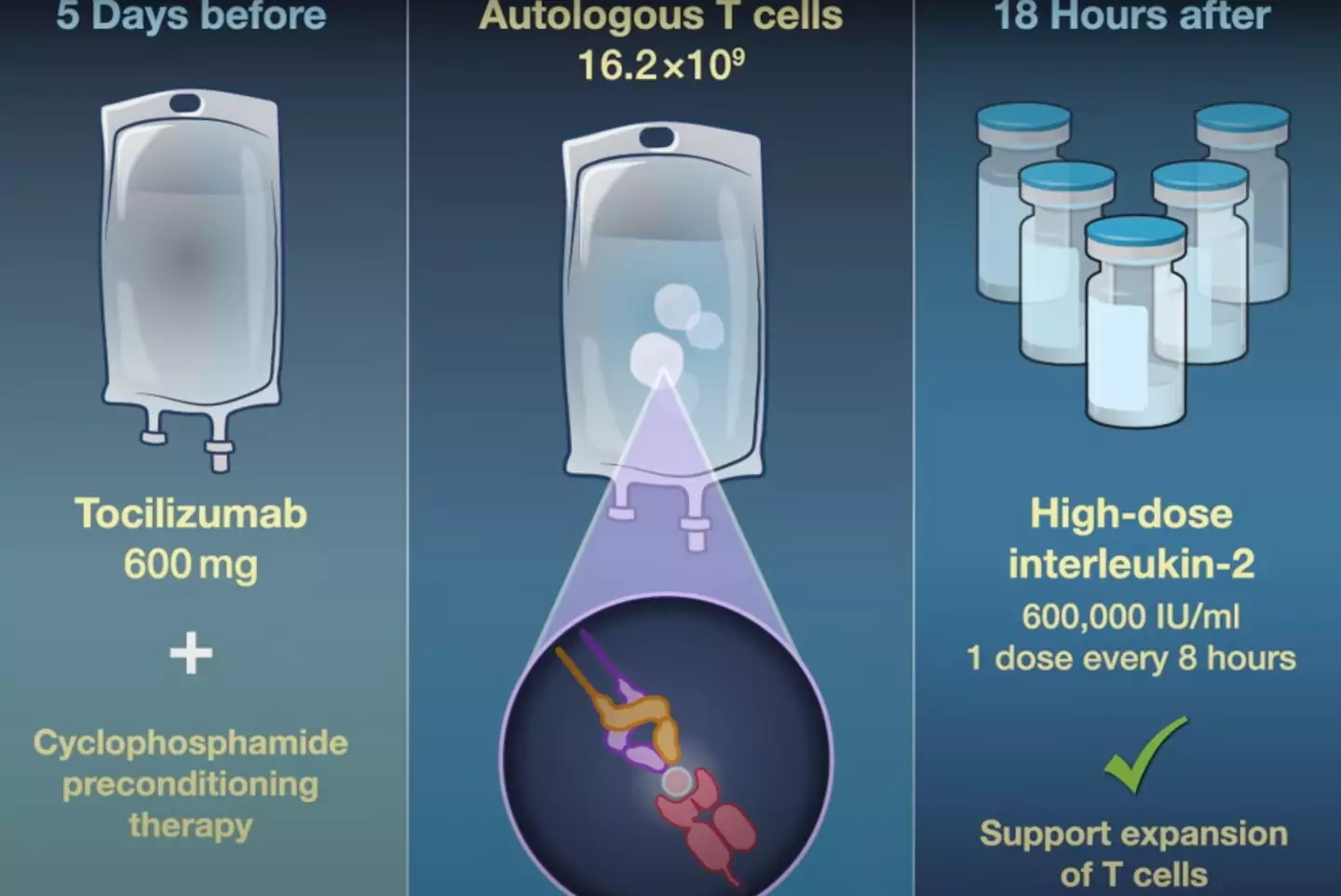
After 11 days, Wilkes was discharged from hospital and she continued her treatment as an outpatient.
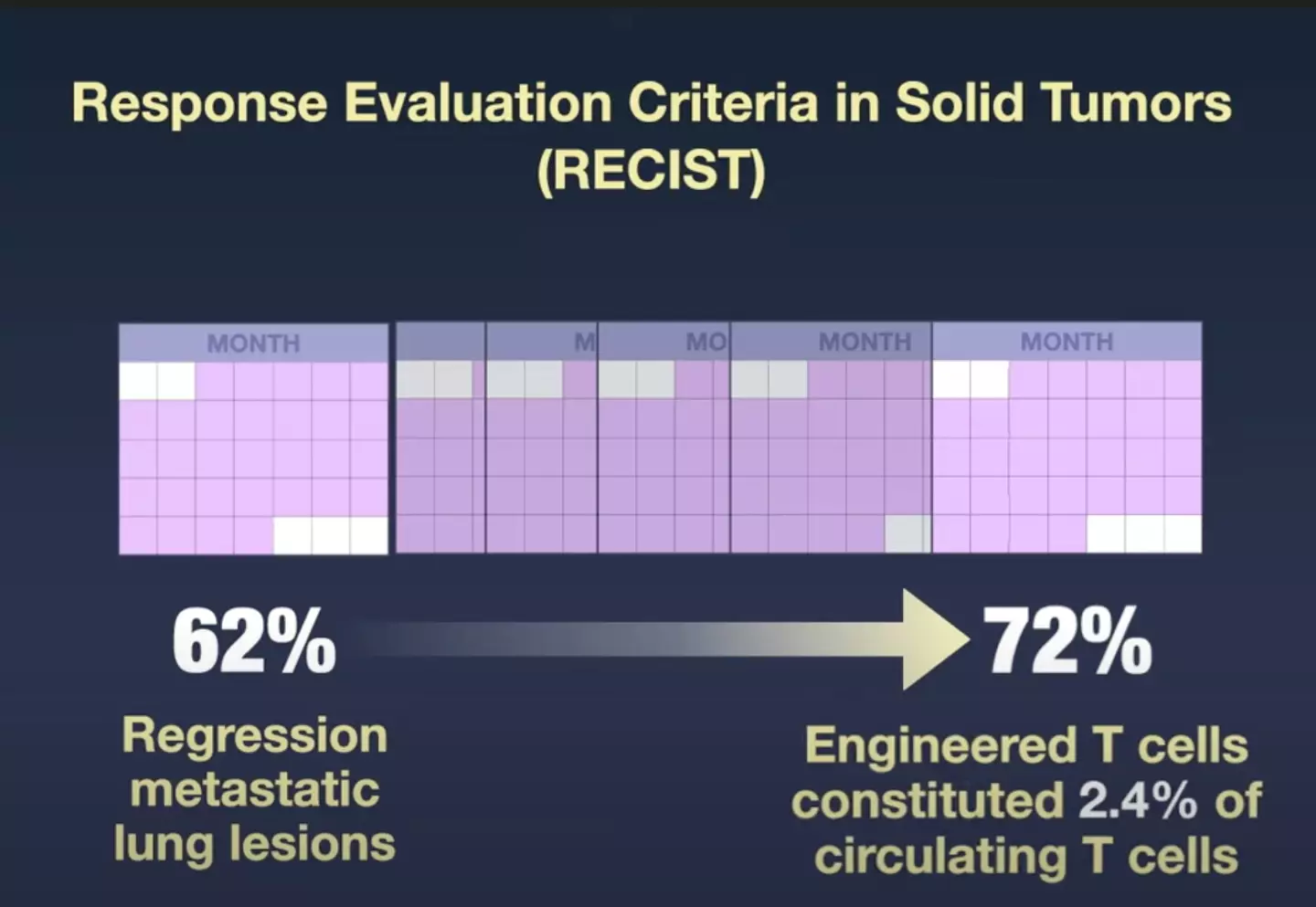
In just one month, Wilkes' metastic cancer was revealed as having shrunk by half.
Advert
The report stated: "Regression of the patient’s metastatic lung lesions was observed on computed tomography at the first clinical follow-up 1 month after the cell infusion, with an overall objective partial response according to the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1, of 62%."
Six months after the treatment, her tumours had reduced by 72 percent.
Pancreatic cancer is one of the most deadly forms of cancer.
Advert
In the UK, there are an average of 10,452 cases every year and 9,558 deaths, giving a survival rate of five percent for surviving the cancer for 10 or more years in England and Wales.
In the US, it is estimated that 'about 62,210 people will be diagnosed with pancreatic cancer' in 2022.
"About 49,830 people will die of pancreatic cancer," American Cancer Society continues.
The experimental therapy is currently only able to be carried out on four per cent of pancreatic cancer patients, as only that amount have a specific molecule required on the cell surface as well as the specific mutation.
However, pancreatic cancer is not the only form of cancer that is known to have such a mutation.
In a media briefing held on Wednesday, 1 June, New England Journal of Medicine's editor-in-chief Dr Eric Rubin stated: "This particular mutation is common in tumors that arise from epithelial cells, such as lung, ovarian and pancreatic cancers.
"We for the first time have an approach that could allow the treatment of a large variety of tumors beyond the small number of tumors that CAR-T cells can be used in a very specific type of immunotherapy."
While Wilkes' reaction to the treatment has been successful and her cancer remains stable, a second patient sadly passed away six months after receiving it.
'Despite high levels of T-cell persistence in the blood, the patient had progressive disease and died 6 months after receipt of the therapy," the report stated.
Pancreatic cancer expert at the Mayo Clinic in Rochester, Minnesota, Dr Ryan Carr suggested Wilkes' positive case may have been down to her cancer having spread to her lungs opposed to her liver – the liver being a more common site of metastasis.
Dr Tran reflected: "We are working hard on trying to answer that question. If we understand the mechanism, that could help us develop better therapies."
Dr Rubin echoed that the experimental treatment has 'encouraging result[s]' but is 'certainly far from a cure'.
To continue investigating the therapy, a Phase One clinical trial is being conducted. The study's authors are subsequently on the look out for patients to recruit.
The study, titled 'Neoantigen T-Cell Receptor Gene Therapy In Pancreatic Cancer' was first published in the New England Journal of Medicine on Wednesday, 1 June.
If you’ve been affected by any of these issues and want to speak to someone in confidence, contact Macmillan’s Cancer Support Line on 0808 808 00 00, 8am–8pm seven days a week